Abstract
Introduction: Fractures of medial condyle of femur are typically rare here we report a case of medial femoral condyle fracture with multiplanar displacement treated with cortico-cancellous screw for compression and posterior tibial plate used as an anti-glide plate/buttress for oblique/spiral configuration of fracture.
Case Presentation: A 78-year-old woman sustained trauma due to fall from stairs and was brought to our hospital with severe right knee pain and inability to bear weight and walk. Knee radiographs (Figure 1) revealed right femoral medial fracture in spiral configuration extending into intercondylar notch as well as breaking in posterior cortex. It is classified (AO classification 33-B2) Patient was initially stabilised and immobilised in splintage. All pre anaesthetic investigations performed and patient was planned for open reduction internal fixation. ORIF was done using two 6.5 mm partially threaded cancellous lag screws to compress the condyle and posteriorly extending oblique pattern of fracture compressed by proximal tibia posterior plate as anti-glide plate. The patient had uneventful post-operative recovery and recent follow up patient achieved a range of motion of zero to 120 degree and could walk without pain.
Conclusion: The locking compression plate for proximal tibia can be used solution for difficult femoral condyle fracture used in reversed position. However careful patient selection is important.
Introduction
Distal femur fractures account for 7% of all femur fractures if hip fractures are excluded then one third of femur fractures involve the distal portion [1], a bimodal age distribution exists with high incidence in young males due to high energy trauma such as motor vehicle or motorcycle accidents or fall from heights a second peak in elderly woman from minor falls there is ratio of 1:2 in men to women [1,2]. Femoral medial condyle fracture (AO classification 33-B2) is a considerably rare fracture. Limited literature is available to give clear view regarding treatment of this fracture configuration. Being metaphyseal region and intra-articular extension, anatomical reduction, and compression as well as stable fixation is a primary necessity to achieve better functional outcome [3]. However, in this case the spiral fracture pattern in distal femur metaphysic the fracture line itself has extended into two planes, Proximal fracture pattern was in coronal orientation and distal in sagittal plane. Hence compression could only have been achieved when screws are placed in the tangential plane to the plane of fracture line. Proximal end of the fracture being smaller in dimension to accommodate the lag screw. However, this compression in other plane could not be achieved through single plane orientation of the plate hence needs isolated another fixation modality. The plate must be precontoured to match posterior surface of distal femur to offer adequate compression till healing and combination construct was needed to be used. Considering the vertical line of fractures and the obliquity of the displacement, screw fixation compression can be done but to achieve stability however no current anatomical plates fit the femoral medial condyle [4,5]. We present a case of femoral medial condyle fracture treated with cancellous screws and posterior tibial plate used as anti-glide plate/buttress plate.
Case Presentation
A 78-year-old woman was brought to our hospital after sustaining trauma to her right knee due to fall from stairs. She was not suffering from chronic neurological illnesses. Parkinson’s disease or stroke or paralysis any signs of central nervous dysfunction or paralyses, all her vital signs were normal. On evaluation patient complained of pain and inability to move right lower limb, there was swelling and bruising over the knee, tenderness was elicited on palpation, distal neurology and vascularity were intact radiographs was done which demonstrated (Figure 1) a femoral medial condyle fracture of right side, the fracture was intra articular and simple oblique through the intercondylar notch (AO classification 33-B2) patient was admitted to our hospital for open reduction internal fixation to be performed following day after stabilization.

Figure 1: radiograph done at time of presentation
Surgical Procedure
Patient was planned for open reduction and internal fixation, under all aseptic conditions, spinal and epidural anaesthesia, fixation patient was performed in supine position. Medial subvastus approach (Figure 2) was used, this approach is used for intra articular fractures of medial condyle of femur, medial Hoffa or in addition to lateral parapatellar approach in case of severe bicondylar articular fragmentation, a skin incision was started at the adductor tubercle and extends proximally just posterior to vastus medialis and the interval between vastus medialis and sartorius was identified, vastus medialis was elevated to expose the medial femoral condyle (Figure 2) the popliteal vascular bundle was protected which lies between adductor Magnus and intermuscular septum.
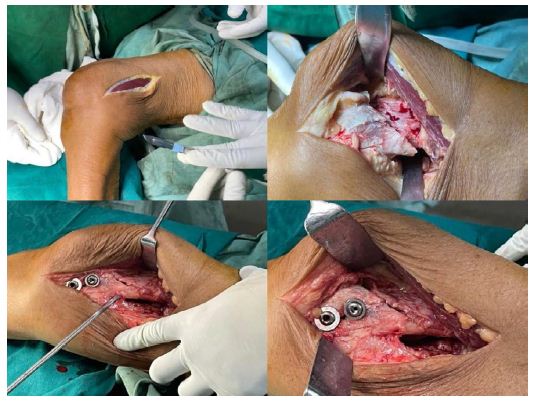
Figure 2: intra-operative images
The fracture was initially compressed with cortico-cancellous screw in coronal plane (Figure 3) and a lag screw was passed to compress the fracture in sagittal plane and then posterior tibial plate was used upside down to fit the Bony surface, the plate was bent for achieving proper anatomical orientation and fixed with cortical and locking screws thus the plate was used as anti-glide/Buttress as per the configuration of the fracture, closure was done in layers. Patient had uneventful post-operative recovery, range of motion exercises were started on Day 1, the weight bearing protocol was toe touch gate for first 4 weeks, by 4th week partial weight bearing from 6 weeks half partial weight bearing and from eight weeks full weight bearing, at the latest follow up the patient had range of motion of zero to 120 degree without any pain, she could walk freely and joint surface restoration was maintained radiologically (Figure 4).

Figure 3: Range of motion after 6 months of surgery

Figure 4: follow up radiograph
Discussion
In elderly patients with osteoporosis a low energy trauma causes simple spiral or oblique fractures the shape of distal femur when viewed end on is a trapezoid with posterior part wide then the anterior part creating 25 degree of inclination on the middle surface and about 10 degree on the lateral surface the plate should lie flat on this lateral surface [6,7], a line that is drawn from anterior aspect of the lateral femoral condyle to the anterior aspect of the medial femoral condyle patellofemoral inclination slopes posteriorly approximately 10 degrees [8,9] this anatomical details are important when inserting any implant or plates, knowledge of the normal radiographic joint line angle helps to assess alignment during an operation the normal anatomical axis of femoral shaft relative to the knee or the anatomical lateral distal femoral angle(LDFA) is 80 to 84 degrees. Measured contralateral lateral distal femoral angle (LDFA) can be used for reference as assessment of coronal alignment, there is consistent pattern of mismatch at the proximal part of the 11-hole locking compression plate for distal femur that may cause valgus malalignment [10].
The quadriceps hamstring and the adductor muscle groups cause significant shortening and varus displacement especially when there are multiple fragments in the metaphysis, the gastrocnemius muscle originates from the posterior aspect of both femoral condyle and its unopposed action causes of flexion deformity of the distal fragment the typical deformity is of shortening with the proximal fragment displaced anteriorly piercing the quadriceps, sometimes the skin while the distal fragment is flexed in varus and rotated posteriorly.
In elderly patients with osteoporosis or Peri-prosthetic distal femoral fractures locking plate systems become valuable for solid fixation [11,12] in situations where there is limited bold stock in the distal fragment the basic principle in treating intra articular distal femoral fractures is based upon anatomical reduction of articular fragments under direct vision fixation is achieved by compressing the fragments with lag screws may be used when required.
However, there are no available anatomical plates that fit either the femoral medial condyle or for fracture fixation, except for the relatively short plate developed for digital femoral Osteotomy [13]. Past reports have shown possibility of screw fixation for the fracture. To date however no consensus exists regarding optimal implant due to very few cases [14]. We used 6.5 mm cancellous screw for compression of femoral condyles. 3.5 mm medial tibia locking plating in reverse mode is used for the same side as anti-glide plate to counteract the vertical and shearing forces. The plate fits the bone surface well after some level of bending. The clinical and radiological outcomes were acceptable the anatomical plate for distal femoral medial condyle should be considered for development as soon as possible.
Conclusion
In our case we used proximal tibial posterior plate upside down as a anti glide plate/Buttress for fixation of femoral medial condyle fracture although the plate needed bending to achieve congruence, it fit well and has yielded glued good clinical outcome the posterior tibial plate could become the method of choice for such fractures.
Funding
Nil
Conflict of interest
Nil
References
- Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37: 691-697. [crossref]
- Ehlinger M, Ducrot G, Adam P, Bonnomet F (2013) Distal femur fractures. Surgical techniques and a review of the literature, Orthop Traumatol Surg Res 99: 353-360. [crossref]
- Bel JC, Court C, Cogan A, Chantelot C, Pietu G, et al. (2014) Unicondylar fractures of the distal femur. Orthop Traumatol Surg Res 100: 873-877. [crossref]
- Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, et al. (2018) For the SCARE Group, The SCARE 2018 statement: updating consensus surgical case report (SCARE) guidelines. Int J Surg 60: 132-136. [crossref]
- Gwathmey Jr. FW, Jones-Quaidoo SM, Kahler D, Hurwitz S, Cui Q (2010) Distal femoral fractures: current concepts. J Am Acad Orthop Surg 18: 597-607. [crossref]
- Murphy CG, Chrea B, Molloy AP, Nicholson P (2013) Small is challenging; distal femur fracture management in an elderly lady with achondroplastic dwarfism. BMJ Case Rep [crossref]
- Manfredini M, Gildone A, Ferrante R, Bernasconi S, Massari L (2001) Unicondylar femoral fractures: therapeutic strategy and long-term results. A review of 23 patients. Acta Orthop Belg 67: 132-138. [crossref]
- Dhillon MS, Mootha AK, Bali K, Prabhakar S, Dhatt SS, et al. (2012) Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literature. Musculoskelet Surg 96 49-54. [crossref]
- Kiyono M, Noda T, Nagano H, Maehara T, Yamakawa Y, et al. (2019) Clinical outcomes of treatment with locking compression plates for distal femoral fractures in a retrospective cohort. J Orthop Surg Res 14: 384. [crossref]
- mcdonald TC, Lambert JJ, Hulick RM, Graves ML, Russell GV, et al. (2019) Treatment of distal femur fractures with the depuy-Synthes variable angle locking compression plate. J Orthop Trauma 33: 432-437.
- Gahlot N, Saini UC, Ss S, Aggarwal S. (2014) Triplane fracture of distal femur in an adult rare case study and review. Ortop Traumatol Rehabil 16: 523-30. [crossref]
- Neer CS, Grantham SA, Shelton ML (1967) Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am 49: 591-613. [crossref]
- Seinsheimer F (1980) Fractures of the distal femur. Clin Orthop Relat Res 153: 169-179.
- Müller ME, Allgöwer M, Schneider R, Willenegger H (1991) Manual of Internal Fixation. Springer, New York.