DOI: 10.31038/SRR.2019211
Summary
Purpose and study design: The research aims to estimate the prevalence and characteristic symptoms of vocal fatigue in professional opera singers. Also, the paper is summary of many years of clinical experience with management of singers with vocal fatigue in Clarós Clinic. The research was designed as a retrospective observational study.
Material and method: In the group of 250 professional opera singers who were examined in Clarós Clinic in 10 years period, fifty-five cases of vocal fatigue were reported and evaluated. Among subjects were 21 men and 34 women. Mean age of participants was 46,78y (range 19–72 years old, standard deviation: 12.18 year). Representation of classical voice types was: 14 tenors, 5 baritones, 2 basses, 22 sopranos, 10 mezzos, 2 contralti.
Results: Prevalence of vocal fatigue in 10 years period in the study group was 22%. The three most frequent symptoms observed in the study group were: muscle pain (87.27%), muscle fatigue (76.36%) and diffuse sharp pain in the neck (70.37%). Statistical analysis showed significance only for the relationship between female opera singers and incidence of symptoms such as tremulous voice and muscle pain. All other symptoms were not statistically related to gender. Contradictory to expectations, application of anti-inflammatory drugs was statistically associated with the longer duration of the symptoms.
Conclusions: Vocal fatigue may be underestimated but is one of the most frequent problems encountered in the ENT practice that provides care for professional voice users. In the presented research, administration of anti-inflammatory drugs has not been associated with faster recovery from vocal fatigue.
Keywords
vocal fatigue, opera singers, treatment of vocal fatigue, retrospective observational study, the prevalence of vocal fatigue.
Introduction
Professional opera singers are considered to be the highest class artists among singers. In fact, they should be perceived as Olympian athletes when comes to quality and ability of their vocal folds. Exceptional singing is achieved by years of training and vocal regime. Unfortunately, the requirements set for the opera singers’ voice entail the unique susceptibility to vocal fatigue. The research reported fatigue to be a common complaint among professional voice users [1].
Vocal fatigue presents a challenge to research and clinical practice. Despite the amount data gathered on that matter, precise definition and guidelines are still not well established.
Unlike in case of muscle fatigue, the creation of the conditions that allow the investigation be far more difficult because of complicated mechanism of voice production. Many studies which attempted to induce vocal fatigue yielded a different and inconsistent result. In case of singing, the task is especially challenging because repertoire can vary significantly. Furthermore, aspect like frequency of the performance can play a role in the development of vocal fatigue. Some types of voice are particularly vulnerable, like a soprano. However, the data provided on the subject is anecdotal, obtained from clinicians’ experience instead of large case-control studies.
Mechanisms which underlay vocal fatigue are multifaceted. Titze listed some potential physiological and biomechanical factors that may contribute: fatigue of respiratory and laryngeal muscles, fatigue of non-muscular tissues of the larynx, and changes in vocal folds’ viscosity [2]. As one of the others, the neuromuscular fatigue express inability of muscles to sustain the tension under repeated stimulation [3].
The exceptional ability of the larynx to produce sound is possible because of vocal folds which are covered with non-muscular, pliable tissue that generates multiple and rapid vibrations [4]. Furthermore, viscous properties of vocal folds epithelium allow lubrication and shock absorption [5]. Research showed that prolonged, high-pitched phonation could increase: frictional energy loss, heat dissipation and tissue viscosity. All these factors can lead to tissue fatigue [4]. The influence of tissue biomechanics on phonation makes the study about vocal fatigue more complicated than the research of fatigue involving other skeletal muscles.
The expression vocal fatigue has been applied and arbitrarily understood. For presented research, vocal fatigue definition was employed from Solomon as the self- report of an increased sense of effort with prolonged phonation, whether or not there are observable or measurable decrements in phonation function [5]. The aspect of self-reporting is particularly crucial amid opera singers who are the harshest judges of their vocal abilities.
Moreover, vocal fatigue has been described clinically by several authors. Common symptoms enlisted in literature were: husky vocal quality, breathy vocal quality, loss of voice, pitch breaks, inability to maintain regular pitch, reduce pitch range, lack of vocal carrying power, reduce loudness range, need to use greater vocal effort [1].
Opera singers are interesting subjects to study vocal fatigue because in comparison to other professional types of vocalists their vocal abilities are challenged at the highest level. Furthermore, years of vocal regime provide them with high self-awareness of the vocal capabilities which helps to notice any vocal problems at first onset.
Clarós Clinic provides medical support for a large number of professional opera singers of Liceu Opera theatre in Barcelona, Music Conservatory students and other singers since 1970’. Authors decided to analyse reports of vocal fatigue from last ten years among opera singers and describe common symptoms, frequency and interventions that were applied.
The research aims to determine the prevalence of vocal fatigue, symptoms and factors which may underlay the occurrence of that problem.
Paper is summary of our experience with treatment and management of vocal fatigue among professional opera singers.
Overall, vocal fatigue is still an intriguing and persistent problem when presented in clinical practice and is the challenge in the face of consequences which may cause for the professional singer with a tight schedule. Furthermore, the struggle with finding a substitute for a famous singer who suffers from vocal fatigue provides additional pressure for the clinician who has to offer effective treatment.
Materials and Methods
Study design
The research was designed as a retrospective observational study. Evaluation of vocal fatigue cases presented in Clarós Clinic during ten years period was conducted to obtain prevalence, symptoms and to analyse the treatment.
The research protocol was approved by ethics committee of Clarós Clinic medical centre.
Participants
In the group of 250 professional opera singers who were treated in Clarós Clinic in 10 years, fifty-five cases of vocal fatigue were reported and evaluated for this research. Among subjects were 21 men and 34 women. Mean age of participants was 46,78y (range 19–72 years old, standard deviation: 12.18 year). Representation of voice types was: 14 tenors, 5 baritones, 2 basses, 22 sopranos, 10 mezzos, 2 contralti.
Medical evidence
Eleven most common symptoms and six risk factors of vocal fatigue identified in the study group were gathered in Table 1.
Table 1. Common symptoms of vocal fatigue and risk factors with definitions.
|
Symptoms
|
Description
|
|
Hoarseness
|
Patient complains of hoarse voice
|
|
Breathy voice
|
Breathy vocal quality, running out of breath while talking
|
|
Whispery voice
|
Patient is only able to whisper
|
|
Tremulous voice
|
Unsteady voice, voice affected by trembling or tremors
|
|
Neck muscle pain
|
Patient complains of muscular pain in the neck
|
|
Sharp pain localised on the neck: diffused or localised
|
Patient complains of sharp pain in the neck during speaking or singing
|
|
Neck muscle fatigue
|
Muscular fatigue present on the neck
|
|
Tissue fatigue
|
Increased viscosity of vocal folds’ mucosa and tissue stiffness
|
|
Neck strain
|
Increased tension in the neck
|
|
Stiffness of the vocal folds
|
Increased tension of vocal folds
|
|
Changes in vibrato
|
Inability to maintain proper vibrato
|
|
Risk factors
|
|
|
Muscle overstrained
|
Excessive effort during performance
|
|
Overuse of voice
|
Inadequate vocal rest regime
|
|
Incorrect technique
|
Insufficient training
|
|
Singing warm-up
|
Inappropriate singing warm-up
|
|
Shouting
|
High-pitched, forced phonation in short period
|
|
Inadequate repertoire
|
Prolonged singing beyond the appropriate tessitura (most acceptable and comfortable vocal range for the given singer [28])
|
Medical records were evaluated to search for possible causes and factor which may contribute to the development of vocal fatigue. Patients reported: overuse of voice, stress, incorrect technique, vocal warm-up, improper repertoire and shouting. Interventions which were used: voice rest regime, medications (anti-inflammatory drugs, steroids: hydrocortisone). Also, duration of the symptoms was measured. In some cases, the repetitive character of vocal fatigue was noticed.
All cases of professional opera singers were presented to the same, senior, most experienced ENT consultant. He was responsible for the patient examination and evaluation. All medical records of patients with vocal fatigue were created by the senior consultant who followed the similar protocol in every case. Table 1 gathers the common symptoms and risk factors assessed in the study with the description of researcher interpretation.
In every case, the standard medical interview was gathered. Moreover, patients underwent ENT examination consisted of endoscopic evaluation and neck palpation.
A senior most experienced ENT consultant performed video laryngoscopy with conventional equipment to examine the vocal folds (Karl Storz® 70 degrees rigid endoscope and HD camera).
The table below shows typical symptoms and risk factors which were assessed in medical records. Description represents how researcher stated or understood given symptom or risk factor. Definitions were based on literature and authors experienced [3,6].
Statistical Analysis
Data was collected in Excel sheet and implemented to Statistica 13.1 (Statsoft) software for statistical analysis. Statistical significance was accepted at the alpha level of 0.05. A p-value below 0.05 was considered significant.
Contingency tables were used to analyse quality variable obtained from patients’ medical history. Percentage values for every symptom and risk factor were calculated for men, women and the complete group. The Chi2 test was used to assess statistical dependence between gender and incidence of given symptom and risk factor.
Contingency tables were also implemented to analyse the possible influence of anti-inflammatory medication on the duration of symptoms.
Due to the qualitative nature of the data obtained from medical history more complicated analyses were not possible.
It needs to be to highlight that some types of voice are very infrequent which influence the precision of statistical analysis. In this study, the contralti, basses and countertenors occurred in the minority.
Results
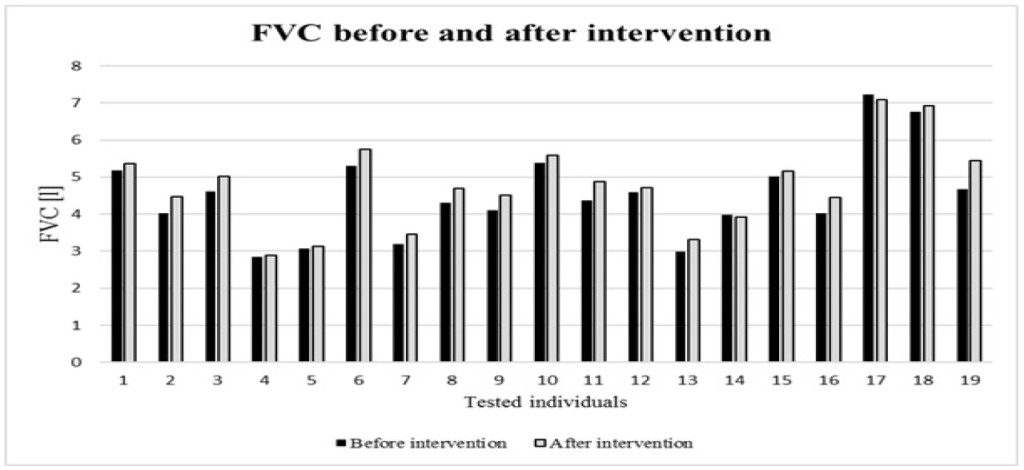
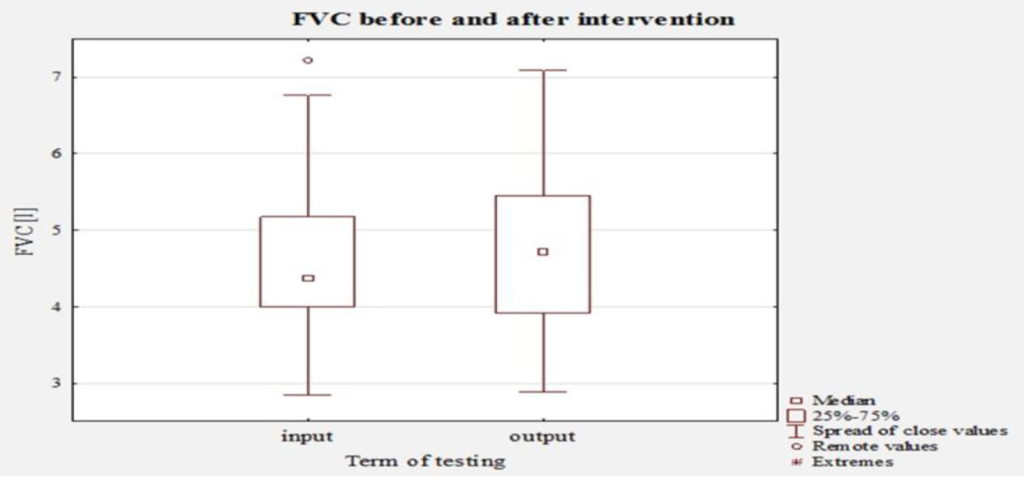
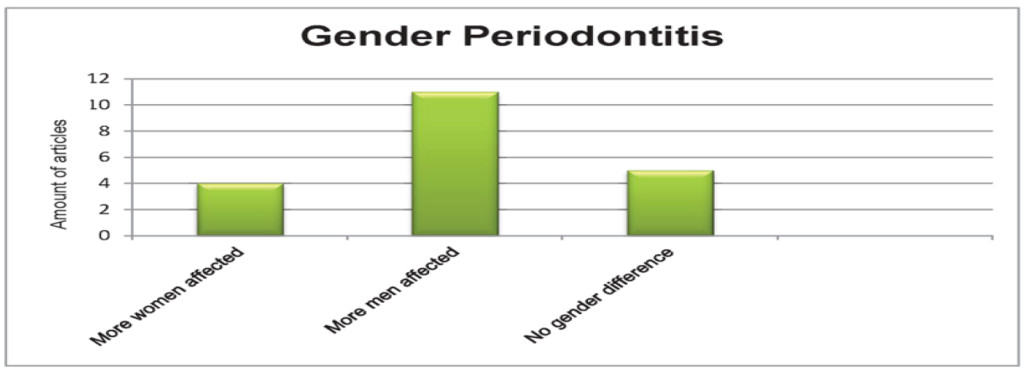
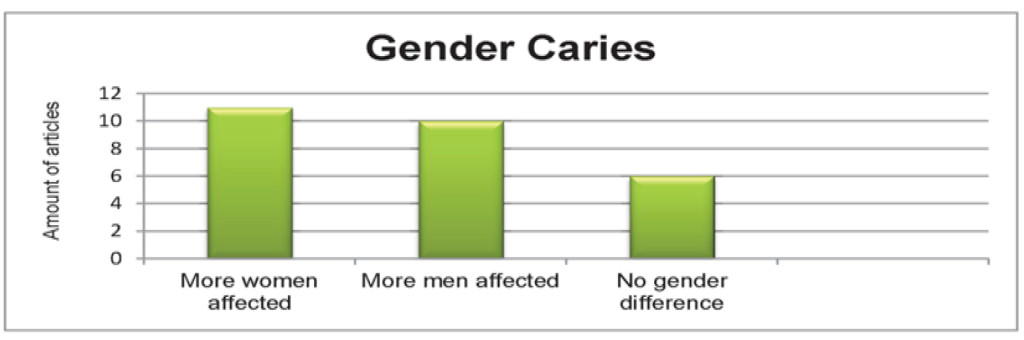
The results section is divided into two parts: descriptive data (tables and chart) and the statistical analysis. The precise characteristic of descriptive data obtained from medical history is presented in table 2, 3 and 4. Percentage values of symptoms incidence are illustrated in Chart 1.

Chart 1. Bar chart. Percentage value of symptoms’ incidence.
Table 2.
Common symptoms of vocal fatigue in the study group.
|
|
Whispery voice
|
Tremulous voice
|
Hoarseness
|
Muscle pain
|
Sharp pain
|
Muscle fatigue
|
Tissue fatigue
|
Vocal folds stiffness
|
Vibrato changes
|
Pitch changes
|
|
|
Diffuse
|
Localised
|
|
|
Men
|
18.18%
|
5.45%
|
21.82%
|
38.18%
|
23.63%
|
7.41%
|
32.73%
|
12.73%
|
23.64%
|
9.09%
|
9.09%
|
|
Women
|
45.45%
|
25.45%
|
40.00%
|
49.09%
|
40.74%
|
22.22%
|
43.64%
|
20.00%
|
27.27%
|
43.64%
|
12.73%
|
|
General
|
63.64%
|
30.91%
|
61.82%
|
87.27%
|
70.37%
|
29.63%
|
76.36%
|
32.73%
|
50.91%
|
52.73%
|
21.82%
|
|
Chi2*
|
p = 0.052
|
p = 0.037
|
p = 0.574
|
p = 0.026
|
p = 0.23
|
p = 0.19
|
p = 0.93
|
p = 0.19
|
p = 0.779
|
p = 0.000
|
|
*The Chi2 for Independence test. Significant values (p≤0.05). NOTE: VF- vocal fatigue.
|
The table shows the percentage of VF occurrence and percentage of cases in which medications were applied in the groups. The results of the Chi2 test for independence between enlisted factor and gender are also given. Significance was reported at p-level below 0.05. None of given factors had gender predilection in the presented group.
Table 3. Risk factors of vocal fatigue analysed in the study group.
|
|
Muscle overstrain
|
Overuse of voice
|
Incorrect technique
|
Singing warm-up
|
Shouting
|
Inadequate repertoire
|
Reoccurrence VF
|
Medication
|
|
Men
|
32.73%
|
30.91%
|
3.64%
|
18.18%
|
20.00%
|
10.91%
|
7.27%
|
10.91%
|
|
Women
|
49.09%
|
49.09%
|
10.91%
|
21.82%
|
29.09%
|
18.18%
|
23.65%
|
14.55%
|
|
General
|
81.82%
|
80.00%
|
14.55%
|
40%
|
49.09%
|
29.09%
|
30.91%
|
25.24%
|
|
Chi2*
|
p = 0.55
|
p = 0.889
|
p = 0.406
|
p = 0.34
|
p = 0.7
|
p = 0.946
|
p = 0.13
|
p = 0.676
|
|
*The Chi2 for Independence test. Significant values (p ≤ 0.05). NOTE: VF- vocal fatigue.
|
The table shows the percentage value of risk factors incidence in the groups and results of the Chi2 test for independence between enlisted factor and gender. Significance was reported at p-level below 0.05. None of given risk factors had gender predilection in the presented group.
Table 4. Percentage value of vocal fatigue reoccurrence. Percentage of cases in which anti-inflammatory medication was applied.
|
|
Reoccurrence VF
|
Medication
|
|
Men
|
7.27%
|
10.91%
|
|
Women
|
23.65%
|
14.55%
|
|
General
|
30.91%
|
25.24%
|
|
Chi2*
|
p=0.13
|
p=0.676
|
|
*The Chi2 for Independence test. Significant values (p≤0.05). NOTE: VF- vocal fatigue.
|
The Chi2 for Independence test was used to assess the relationship between gender and vocal fatigue symptoms. Results of the Chi2 test are also given in tables 2, 3.
Table 5 presents the percentage values of vocal fatigue recurrence among different types of classical voices.
Table 5. Recurrence of vocal fatigue among different voice types (tessitura- defined as most acceptable and comfortable vocal range for the given singer [28]).
|
Recurrence of vocal fatigue in different voice types
|
|
|
Yes
|
No
|
General
|
|
Soprano
|
12.73%
|
27.27%
|
40.00%
|
|
Mezzosoprano
|
10.91%
|
7.27%
|
18.18%
|
|
Contralto
|
0,00%
|
3.64%
|
3.64%
|
|
Tenor
|
5.45%
|
20.00%
|
25.45%
|
|
Baritone
|
1.82%
|
7.27%
|
9.09%
|
|
Bass
|
0.00%
|
3.64%
|
3.64%
|
|
General
|
30.91%
|
69.09%
|
100.00%
|
The table shows the percentage value of risk factors incidence in the groups and results of the Chi2 test for independence between enlisted factor and gender. Significance was reported at p-level below 0.05. None of given risk factors had gender predilection in the presented group.
The table presents the percentage of vocal fatigue reoccurrence among different voice types. In presented data sopranos and tenors were most frequently affected by the reoccurrence of VF. Examined contralti and basses had not experienced vocal fatigue more than one time at the moment of evaluation.
The chart shows the percentage value of symptoms which occurred in the whole group (general), men and women groups. Bars help to illustrate which symptoms were most common and compared them between groups. Therefore, three most frequent symptoms were muscle fatigue, diffuse sharp pain and muscle pain. Most common symptom among women as well as in men was muscle pain.
Results – Summary
The Clarós Clinic provided medical support for 250 professional opera singers during the time that the data was gathered. Symptoms of vocal fatigue were reported in 55 operatic vocalists, and these cases were enlisted to the research.
Prevalence of vocal fatigue in 10 years period among opera singers examined in the Clinic was 22%.
The three most frequent symptoms observed in the study group were: muscle pain (87.27%), muscle fatigue (76.36%) and diffuse sharp pain (70.37%). Most frequent complaints were pain-related, especially in female singers group.
Most common vocal complaints were: whispery voice (63.64%) and hoarseness (61.82%). More than a half of opera singers (52.73%) had difficulties with maintaining the vocal pitch during singing and quarter (21.82%) noticed changes in vibrato
The Chi2 test showed statistical significance only for the relationship between female opera singers and incidence of symptoms such as tremulous voice and muscle pain (test Chi2: p = 0.037, p = 0.026). All other symptoms were not statistically related to gender.
Most common risk factors were: muscle overstain and overuse of voice which were present in over 80% of cases. Much less frequently, singers reported incorrect technique and inadequate repertoire as contributors to vocal fatigue (table 3).
Recurrence of vocal fatigue was noted in one-third of the singers and was more distinctive for female singers, especially sopranos and mezzo-sopranos (table 4).
Mean duration of the symptoms was 3.8day (standard deviation: +/- 1.9day). The median value was 3 day.
Contingency tables were also used to estimate the relationship between duration of the symptoms and application of anti-inflammatory medications. Results of the Chi2 test showed that shorter length of the symptoms was related to lack of administration medication (test Chi2: p = 0.009).
Discussion
Vocal fatigue is an interesting and often debilitating condition, affecting many professional voice users. It gained much attention in the field of research, yet mechanisms which underlie the onset of this condition and its pathophysiology are still not fully understood. The amounts of vocal effort and specific elements which can trigger vocal fatigue are part of the ongoing debate. More research has to be done to develop reliable guidelines for management and treatment of vocal fatigue.
Every group of professional voice users have its characteristic which helps to study individual exposure factors. Opera singers have the individual susceptibility to fatigue which may interfere with social and occupational functioning.
The purpose of this study on vocal fatigue in opera singers was to state prevalence, characterise symptoms of this condition and review management.
Prevalence of vocal fatigue in studied group was 22%, which suggests that it might concern every fifth singer. As previous research showed among other types of professional singers, VF can cause voice impairment even more often. In a study conducted on the large group of various kinds of singers (opera singers- 49.8%), Phyland reported that participants experienced vocal fatigue in the previous year in 69% of cases [7]. In the research, fatigue was the second most frequent problem reported by singers after hoarseness [7].
Among most common symptoms reported by opera singers in the study group: two were pain related. Over 87% of singers pointed out the muscle pain as a single most common symptom of vocal fatigue. Female opera singers tended to suffer more from muscle pain than male singers, which was also confirmed statistically significant. Muscle pain was usually localised in throat, jaw and neck, but also in chest and back. These findings were consistent with previous reports which stated that most common pain present in singers were a sore throat (66%), pain during speaking (41%) and neck pain (35%). However, the study mentioned above pointed out the tendency for a sore throat among male vocalists, other types of body pains had no difference according to gender [8]. The presence of pain can severely compromise singer’s performance and negatively influence the quality of life. An important factor which helps to prevent the muscle pain is the concern for proper technique and vocal rest regimen.
Neuromuscular fatigue has been widely investigated in the literature. It can be presumed that muscle of the respiratory and phonatory system can fatigue and contribute to the deterioration of phonation or the perception of increased vocal effort, especially during prolonged high-pitched phonation. Undoubtedly, the research showed that respiratory muscles are highly unlikely to experienced fatigue. More recent findings presented evidence from whole body exercise suggesting that respiratory muscle fatigue occurs only following constant high-intensity training [9]. This situation cannot occur during regular physical activity, even as challenging as prolonged singing.
The distinction between fatigue of skeletal muscle and phonation muscles is relevant, because of the different histological structure. The capability of a muscle to maintain contraction over an extended period is related to a distribution of different motor units within the muscle body. In case of the larynx, the vast majority of intrinsic laryngeal muscle have fatigue-resistant muscle fibres (type I and IIa) rather than fatigable (type IIb) [10]. More recent studies provide interesting data showing the even more complicated histological structure of human intrinsic laryngeal muscles than presented in animal models [10]. These facts help to explain why singers usually complain about fatigue of muscle and experience discomfort in areas primarily localised in throat, jaw, and neck.
One of the unique aspects is non-muscular tissue fatigue which represents mechanical exhaustion. Mechanical deterioration represents the amount of strain that material can tolerate before breaking down. The fatigue represents progressive structural damage that results from mechanical stress (force per unit) imposed by strain on the material. Titze reported in one of his research that non-muscular tissue fatigue could cause damage to the laryngeal mucosa, but the quantity and duration of the physical stress were uncertain [11]. The author also described tensile stress which is required for high pitch phonation as a most significant mechanical stress in vocal folds vibration [11]
Tissue viscosity plays a role in response to mechanical stress because that feature refers to individual properties of vocal folds’ mucosa responsible for lubrication and shock absorption. Research demonstrated that viscosity highly depends on the systemic and superficial hydration of mucosa. Singers in a situation of reduced systemic hydration may be particularly prone to experience the vocal fatigue [12]. Factor as prolonged, high-pitched phonation without proper hydration can lead to stress and strain which placed on the tissue can provoke fatigue. Furthermore, the viscosity of vocal folds mucosa can be affected by the decreased humidity of environment as in case of oral breathing [13].
The more recent study confirmed positive influence of systemic hydration on perceptual parameters of voice quality in singers. The improvement was seen in higher fundamental frequency, less cycle to cycle variation in pitch, or longer phonation time, depending on the individual. Hydrated vocal folds allow for optimal vibration, increase ease of phonation and prevent structural damage to vocal to vocal folds mucosa [14,15,16].
Non-muscular tissue biomechanical properties which include mucosal viscosity plays a significant role in the development of fatigue. In presented study 1/3 of singers have suffered from problems related to tissue fatigue.
Further, changes in vibrato were observed in over 52% singers. These changes represent acoustic differences related to vocal fatigue and can seriously interfere with performance. In previous research, Titze noted that muscle fatigue results in decreased ability to maintain stable tension in vocal folds [2]. In another interesting study, Boucher attempted to isolate acoustic signs of fatigue in laryngeal muscles. The study showed that 12 conventional acoustic parameters that were measured neither demonstrated consistent linear relationships with the fatigue estimates. Though, average values demonstrated the consistent peaks in vocal tremor and appeared near the points of critical shifts in muscle fatigue. In sum, rises in tremor corresponding to shifts in muscle fatigue appear robust in the face of fluctuations in modal pitch [17].
A more recent study helped to differentiate the acoustic changes related to vocal fatigue. The research was the first to demonstrate a link between tremor and observed muscle fatigue that is specifically attributable to voice effort and not only to fatigue linked with waking hours. Also, the results do not support applications of F0 or other conventional acoustic parameters as manifestations of fatigue in laryngeal structures. Even though many research showed significant rises in F0 as a result of vocal effort with reference to group averages, the recent reports showed that individual or cross-subject changes in F0, as in other conventional acoustic parameters do not consistently indicate fatigue in laryngeal structures [18].
Despite years of research, no consensus has emerged that could support the elaboration of guidelines for vocal fatigue. In the most basic approach, investigations on vocal fatigue have concentrated on identifying changes in voice in tests where fatigue was provoked by tasks of various “vocal load”. The assignments varied across different research; participants were asked to read or sing at varying pitch or intensities for a variable period extending from few minutes to several hours [19]. Those arguments make cross-study comparison useless with results on suggested vocal symptoms inconsistent and sometimes contradictory.
In our study as the first line of treatment, the vocal rest regime was applied in every case. Importance of vocal rest was underlined in many research and is usually required as first line intervention when vocal fatigue is experienced by singer [20]. Stress and anxiety management is also crucial for maintaining the good psychological condition of a singer. The aim of physical and mental approach to prevention of vocal fatigue is optimisation of the performance efficacy [21]. This translate to minimising muscular activation, achievable by improving posture and relaxing muscles [22].
Professional opera singers often follow the vocal routine which usually begins under the influence of their singing teacher and speech-language pathologist. Vocal hygiene practices contain moderation in amount and type of voice use, reduction of stress, avoidance of phonotraumatic behaviours like shouting, talking over crowds, aspects like systemic hydration and humidification to improve performance and ensure voice longevity [23]. Effects of systemic hydration and vocal rest were proved to have a significant influence on the decrease of vocal fatigue and maintaining good vocal quality in general [16,24].
In literature, researchers postulated to set safety limits of vibration dose (phonatory time) for professional voice users to protect people in several occupations (singers, teachers). For instance, proper recovery time has been worked out for professional athletes who abuse their body in different ways. Importantly, Titze divided recovery for short- and long-term. The first one takes place immediately when phonation is stopped [25]. The primary benefit from short recovery is for the muscles whose chemicals get reset before next contractions. On the contrary, traumatised epithelial cells need more prolonged healing. Some of them after being heavily bombarded during vocal folds contraction can degenerate and be shed off. New cells will grow underneath, but that requires time. Furthermore, some destruction of the structural matrix of the lamina propria may be present after prolonged phonation. Fibroblasts activity is necessary for the repairing to continue constantly. The recovery process may range from several hours to 72h to complete [25]. As was presented in the study, the actual phonation for opera singers in 2–3h opera was of the series 20–30min for leading role, and their schedule performance was on the order of 3 per week [25]. Overall, these facts put opera singers in the favourable position for proper vocal recovery. Nevertheless, the type and loudness of phonation were not considered in research calculation, but they can play a tremendous role. Given this points, more research is needed to create appropriate guidelines to prevent singers from vocal fatigue.
Singers appear to be at particular risk of developing voice problems. Formal assessments of singers experiencing a voice problem at any given moment in a time range from about 20 to 50% [26]. Moreover, the impact of voice problems on quality of life was widely investigated in the literature. Many studies proved that decrease in voice quality and other voice impairments affects severely quality of life. Of course, in case of professional singers, this problem grows to the crucial role because directly concerns the source of income.
Attempts at analysing vocal fatigue in patients who already experienced this condition are difficult because of subject heterogeneity and burden with problems of data interpretation. Even individuals selected for having only symptoms of vocal fatigue usually present variable baseline and outcome data.
Professional opera singers have high stakes in sustaining excellent vocal condition but also experienced unique vocal demands, making them important population to study.
Useful tools to adapt to everyday practice are scales which help to evaluate singers’ perceptions of physical aspects of singing status. A good example is EASE scale (Evaluation of the Ability to Sing Easily) which is clinical outcome test for symptomatic aspects of compromised vocal health but was not designed as the primarily disease-specific instrument [27]. This test serves as the measure of potential changes in the singing voice which may indicate effects of vocal effort and may help to detect singers with the increased risk of possible development of voice disorders. The EASE was designed to help singers in assessing vocal load threshold, recovery time to assist performance scheduling, help to predict the development of vocal problems, evaluate therapeutic outcome in management for specific needs of the singer’s voice, lastly to provide supportive data for determining performance fitness [27].
Conclusion
Vocal fatigue may be underestimated but is one of the most frequent problems encountered in the ENT practice which provides care for professional voice users. The most frequent symptoms were muscle fatigue, diffuse sharp pain and muscle pain. In the study group, administration of anti-inflammatory drugs has not been associated with faster recovery from vocal fatigue.
References
- Kitch JA, Oates J (1994) The perceptual features of vocal fatigue as self-reported by a group of actors and singers. J Voice 8: 207–214.
- Titze I.R. (1984) Vocal fatigue: some biomechanical considerations. In: Lawrence VL (ed). (Transcripts of the Twelfth Symposium: Care of the professional voice Part One:Scientific Papers. New York: The Voice. Foundation;) Pg No: 97–104.
- Welham NV, Maclagan MA (2003) Vocal fatigue: current knowledge and future directions. J Voice 17: 21–30. [crossref]
- Cooper DS, Titze IR (1985) Generation and dissipation of heat in vocal fold tissue. J Speech Hear Res 28: 207–215. [crossref]
- Solomon NP (2008) Vocal fatigue and its relation to vocal hyperfunction . Int J Speech Lang Pathol 10: 254–266. [crossref]
- Sataloff RT () Professional Voice: The Science and Art of Clinical Care, 3-Volume Set, Fourth Edition. https://books.google.es/books?id=ImVGDwAAQBAJ&pg=PA547&dq =the+performance+voice+benninger&hl=pl&sa=X&ved= 0ahUKEwiUhqbJlLPZAhWDWxQKHRS7ARIQ6AEIcTAJ#v = onepage&q&f = false. Accessed February 20, 2018.
- Phyland DJ, Oates J, Greenwood KM (1999) Self reported voice problems among three groups of professional singers. 13: 602–611.
- Rocha C1, Moraes M, Behlau M (2012) Pain in popular singers. J Soc Bras Fonoaudiol 24: 374–380. [crossref]
- Faghy MA, Brown PI (2014) Thoracic load carriage-induced respiratory muscle fatigue. Eur J Appl Physiol 114: 1085–1093. [crossref]
- Wu YZ, Crumley RL, Armstrong WB, Caiozzo VJ (2000) New perspectives about human laryngeal muscle: single-fiber analyses and interspecies comparisons. Arch Otolaryngol Head Neck Surg 126: 857.
- Titze IR (1994) Mechanical stress in phonation. J Voice. 8: 99–105.
- Pearl Solomon N, Stemmle DiMattia M (2000) Effects of a vocally fatiguing task and systemic hydration on phonation threshold pressure. J Voice 14: 341–362
- Sivasankar M, Fisher KV (2002) Oral breathing increases Pth and vocal effort by superficial drying of vocal fold mucosa. J Voice 16: 172–181. [crossref]
- van Wyk L, Cloete M, Hattingh D, van der Linde J, Geertsema S (2017) The Effect of Hydration on the Voice Quality of Future Professional Vocal Performers. J Voice 31: 111. [crossref]
- Verdolini K, Min Y, Titze IR, Lemke J, Brown K, et al. (2002) Biological mechanisms underlying voice changes due to dehydration. J Speech Lang Hear Res 45: 268–281. [crossref]
- Leydon C, Wroblewski M, Eichorn N, Sivasankar M (2010) A meta-analysis of outcomes of hydration intervention on phonation threshold pressure. J Voice 24: 637–643.
- Boucher VJ (2008) Acoustic Correlates of Fatigue in Laryngeal Muscles: Findings for a Criterion-Based Prevention of Acquired Voice Pathologies. J Speech Lang Hear Res 51: 1161.
- Boucher VJ, Ayad T (2010) Physiological Attributes of Vocal Fatigue and Their Acoustic Effects: A Synthesis of Findings for a Criterion-Based Prevention of Acquired Voice Disorders. J Voice 24: 324–336.
- Caraty MJ, Montacié C (2014) Vocal fatigue induced by prolonged oral reading: Analysis and detection. Comput Speech Lang 28: 453–466.
- Behlau M, Oliveira G (2009) Vocal hygiene for the voice professional. Curr Opin Otolaryngol Head Neck Surg 17: 149–154. [crossref]
- Boucher VJ, Ahmarani C, Ayad T (2006) Physiologic features of vocal fatigue: Electromyographic spectral-compression in laryngeal muscles. Laryngoscope. 116: 959–965.
- Angsuwarangsee T, Morrison M (2002) Extrinsic laryngeal muscular tension in patients with voice disorders. J Voice 16: 333–343. [crossref]
- Timmermans B1, Vanderwegen J, De Bodt MS (2005) Outcome of vocal hygiene in singers. Curr Opin Otolaryngol Head Neck Surg 13: 138–142. [crossref]
- Yiu EM, Chan RM (2003) Effect of hydration and vocal rest on the vocal fatigue in amateur karaoke singers. J Voice 17: 216–227. [crossref]
- Titze IR (1999) Toward occupational safety criteria for vocalization. Logop Phoniatr Vocology 24: 49–54.
- Verdolini K, Ramig LO (2001) Review: occupational risks for voice problems. Logoped Phoniatr Vocol 26: 37–46. [crossref]
- Phyland DJ, Pallant JF, Benninger MS, et al. (2013) Development and preliminary validation of the EASE: A tool to measure perceived singing voice function. J Voice 27: 454–462.
- Smith B (2013) Choral Pedagogy. In: Brenda J, Sataloff RT (eds). (3rdedn). Plural Publishing, North America: 344.